What’s the true cost of care in Canada?
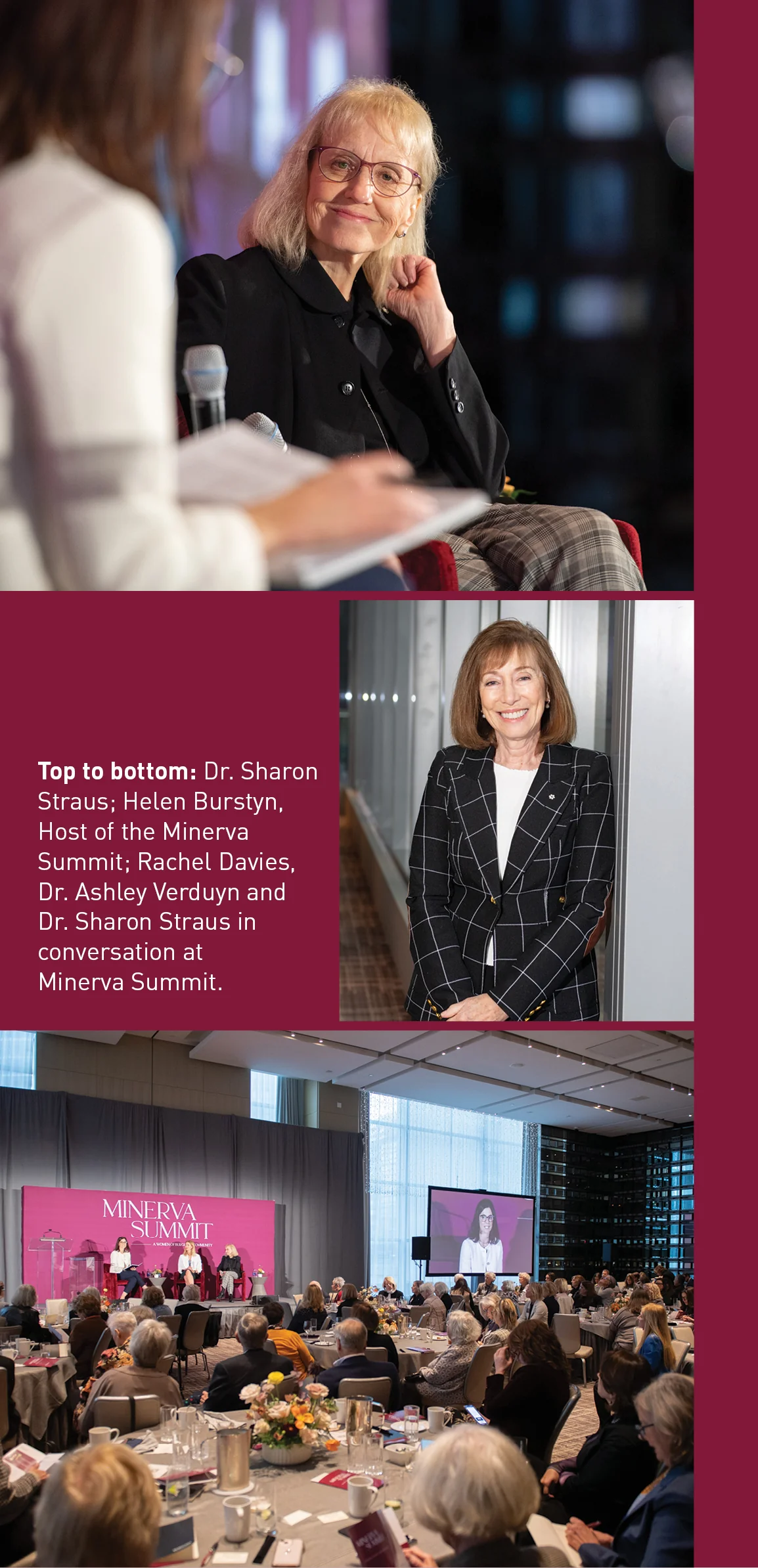
In this candid conversation from Minerva’s latest Summit, Burgundy’s Rachel Davies speaks with two leading voices in Canadian medicine, Dr. Sharon Straus and Dr. Ashley Verduyn, for an inside look at the health-care system. They explore the holistic nature of geriatric care, the critical role of families and caregivers, and the unexpected costs of long-term support. With Canadians facing longer waitlists for primary care and ongoing challenges in accessing specialized services, self-advocacy and financial preparedness are more important than ever.
Rachel Davies: I want to begin by sincerely thanking you both for making time for this important conversation. Among our clients, there’s a strong desire to better understand how the Canadian health-care system works, particularly as we age and require more care. To establish a common understanding, I’d like to start with a question for Dr. Straus: As a renowned geriatrician, could you help us understand the role your specialty plays in our health-care system?
Dr. Sharon Straus: As a geriatrician, I specialize in caring for people aged 65 and older—with one important exception that I’ll explain shortly. Our training path differs from primary-care physicians: After medical school, we complete specialty training in internal medicine, followed by two additional years of subspeciality training focusing on geriatric medicine. We primarily treat patients with complex medical conditions, such as dementia, working closely in partnership with primary-care colleagues. Currently in Canada, there is only half of a geriatrician available for every 10,000 people over 65. To put this shortage in perspective, the number of new geriatricians we train annually is just one-quarter of the number of people who enter cardiology. This creates a significant gap in caring for our aging population.
Geriatric medicine is also a holistic specialty. We address medical, social, and psychological aspects of care. This comprehensive approach is what draws me to the field. We treat the whole person while also involving family members and caregivers in the care plan.
As I mentioned earlier, there is one exception to our age requirement: For people with lived experience of homelessness, we begin care at age 50. This is because homelessness accelerates aging—a 50-year-old who has experienced homelessness is typically equivalent physiologically to someone 20 years older.
RD: Could you explain the different pathways to accessing geriatric care?
SS: Access is available through two main pathways. First, primary-care clinicians can make direct referrals to a geriatrician. Second, we provide consultations within hospitals, which I do across several locations within Unity Health, including Providence and St. Michael’s.
At St. Michael’s, we’ve developed several programs. For example, our Acute Care for the Elderly Unit admits patients over 65 directly from emergency with acute medical issues, focusing on those who can return home, with support, for independence. We’ve also pioneered an innovative trauma-care program where geriatrics automatically consults on every trauma patient aged 65 and older. This program, developed by Dr. Camilla Wong and Dr. Marissa Zorzitto, has significantly improved outcomes for older adults with falls and injuries, and has been adopted by trauma centres across Canada.
“Family physicians and nurse practitioners are crucial for preventative screenings, managing chronic illness, connecting patients to community programs, and facilitating access to specialists, like geriatricians.”
RD: Dr. Verduyn, perhaps like many Canadians, I had assumed our universal health-care system was designed to cover most medical needs, with private insurance mainly handling dental and pharmaceutical coverage. I was surprised to learn that when universal health care was introduced in the 1960s, its primary focus was on ensuring access to family doctors and hospital care. Long-term care wasn’t prioritized because we were a younger nation— at the time, the average Canadian was 26 years old and life expectancy was around 70. Because we didn’t fully understand the health-care needs of an aging population, services had to be added incrementally rather than through a comprehensive design for elder care. This helps to explain why navigating the system can be so challenging as we age. Dr. Verduyn, as Chief of Providence, you work at the intersection of hospitals, rehabilitation, and long-term care. Could you give us an overview of how these different levels of care work together?
Dr. Ashley Verduyn: You’re right, it’s complex. While we’re fortunate to have publicly funded health care, there are significant gaps.
Primary care is the foundation of our system, and it’s currently in crisis. Over five million Canadians lack a primary-care team. Family physicians and nurse practitioners are crucial for preventative screenings, managing chronic illness, connecting patients to community programs, and facilitating access to specialists, like geriatricians.
Our hospitals remain vital for acute-care needs like illness, accidents, and trauma. However, they are increasingly serving as a broader safety net people experiencing social issues like homelessness and a lack of community supports. Rising living costs have led to housing insecurity, resulting in more people seeking hospital services even without acute medical needs.
Following hospitalization, rehabilitation is essential for regaining function, particularly in older adults. Even brief hospital stays can cause muscle weakness that makes it difficult or impossible for patients to stand or walk independently. Fortunately, these vital services are available in hospitals and community settings. Evidence shows that geriatric rehabilitation helps patients regain function, prevent falls, reduce emergency room visits, and maintain independence at home.
Home- and community-care services help transition patients back home. While these services are part of our publicly funded health-care system, they are often quite limited. Support might consist of just one weekly visit from a personal support worker (PSW) for bathing assistance, or occasional nursing care for wound management. Most patients need additional support from personal caregivers to fill significant gaps in care.
Long-term care homes are specifically designed for people requiring 24/7 care from nurses or personal support workers. About 80 percent of long-term care residents in Canada have cognitive impairment, such as dementia or physical disabilities that severely limit their ability to perform daily activities like moving, transferring, or using the washroom independently. These homes also serve adults with complex mental health issues or severe intellectual disabilities requiring around-the-clock care.
Finally, palliative care is a vital part of this health-care continuum. It’s not just a service, but a philosophy of care that can be provided in various settings—from dedicated palliative-care units and hospices to patients’ own homes.
RD: Dr. Straus, Dr. Verduyn touched on several resource limitations and care gaps. From your perspective, what do you see as the most critical gaps in our health-care system today?
SS: There are two major gaps we need to address. First is the critical shortage in primary care and access to fully staffed family-health teams. The second is the challenge of navigating our health-care system. Whether you’re a caregiver or an older adult without support, it’s incredibly difficult to identify and access needed resources. This includes finding help with basic activities of daily living, such as bathing and dressing, as well as more complex tasks like managing finances and arranging transportation to medical appointments. The gap isn’t just in accessing clinical care—it’s in finding and coordinating all of these essential support services.
Another significant gap in our health-care system is support for caregivers. Those of you who have been caregivers know that the stress of caregiving itself becomes a risk factor for health problems. Ensuring caregivers receive proper support and care is crucial, yet remains inadequate.
This connects to our broader challenge of supporting those who cannot live independently. The COVID-19 pandemic exposed serious issues in long-term care facilities. While there’s a natural desire to put the pandemic behind us, I’m concerned we’re overlooking crucial lessons learned during that time. In Ontario, for example, several long-term care homes are now closing because they cannot implement recommended improvements, which will only increase waiting lists for care.
“Those of you who have been caregivers know that the stress of caregiving itself becomes a risk factor for health problems. Ensuring caregivers receive proper support and care is crucial, yet remains inadequate.”
A particularly urgent issue that Ashley and I are passionate about is supporting less resourced populations, especially regarding housing stability. Women are disproportionately affected—they generally live longer, often need more financial support, and are increasingly at risk of becoming precariously housed. Imagine someone hospitalized for an acute illness who misses rent payments and faces eviction—this scenario creates a cascade of health and social challenges that our system struggles to address.
Finally, we need to encourage people to have clear discussions with their families about their wishes. This includes advanced-care planning and designating powers of attorney for both personal care and finances. As clinicians, we emphasize the importance of having these crucial conversations early, before they become urgent. These discussions are far more effective when they happen during calmer times, allowing families to make thoughtful decisions about future care and support.
RD: Dr. Verduyn, what key challenges do you encounter in rehabilitation and long-term care?
AV: A major challenge many don’t anticipate is the cost of medical equipment. Essential items like walkers and wheelchairs come with significant expenses, and this often triggers a cascade of housing modifications. A stair lift alone can cost $15,000—beyond many patients’ means. This financial burden becomes particularly challenging when combined with the rising cost of living. We need to plan how to adapt our environments to accommodate potential future needs for mobility equipment.
Another major gap involves community support for those wanting to age at home. The waiting list for long-term care in Ontario currently stands at about 45,000 people. Supportive housing, where residents live in apartments with embedded PSW services, could help many age in place, but has an even longer waiting list. This gap in community support and affordable supportive housing is leading to increased homelessness among older adults, especially those without family support to help navigate the system.
RD: We know that most people who have stable housing prefer to age in their homes. As family members, how can we assess whether a home environment will safely support our loved ones as they age? And what signs should we watch for that might indicate they need additional support or potentially a transition to more care, while still respecting their independence?
AV: We always strive to honour our patients’ wishes, and you’re right, most people prefer aging at home. Occupational therapy is an invaluable resource in this process. These professionals, available through home- and community-care services, can visit homes and identify potential hazards that most people miss, from tripping hazards to areas needing safety features. Today’s technology also offers more options than ever before, from fall alarms to video monitoring systems that help us check on loved ones, though cost can be a barrier. The greatest challenge typically arises when someone requires 24-hour care. Providing around-the-clock support in a home environment is extraordinarily expensive, making it financially unfeasible for many families.
SS: I’d add an important point about autonomy. As a caregiver for my elderly parents, I’ve learned that we sometimes need to accept choices we disagree with. When my mother chooses not to use her walker, I worry, but I’ve realized that respecting her right to make decisions— even ones I disagree with—is crucial to maintaining her dignity and independence.
 RD: You both mentioned challenges in long-term care that were exposed during COVID-19. As members of the COVID-19 task force, what key insights did you gain about long-term care, and what issues still need our attention?
RD: You both mentioned challenges in long-term care that were exposed during COVID-19. As members of the COVID-19 task force, what key insights did you gain about long-term care, and what issues still need our attention?
SS: This topic is near and dear to our hearts because it’s fundamentally about providing the best possible home environment for older adults who need long-term care. We must remember this crucial point: These facilities aren’t institutions, they’re homes for people who require intensive, direct care.
Current funding doesn’t align with the evidence-based recommendations for direct care hours these residents should receive. We’re not asking for excessive care—just meeting proven, basic needs for our residents. Yet we continue to fall short of these fundamental standards. The staffing situation is equally concerning. Our workforce, predominantly racialized women older than the median Canadian worker, typically earns less than acute-care counterparts unless attached to organizations like Unity Health. This wage disparity reflects a deeper issue: How we value both older adults and those who care for them.
We need strong advocacy to ensure these standards are delivered across Canada. This means pushing for accountability in federal transfer payments to provinces and territories, ensuring the funding directly improves care quality in long-term care homes.
AV: The waiting list situation illustrates these challenges. With a nine- to 10-year wait at our long-term care facility, the system can only accommodate crisis admissions based on scores that evaluate factors such as cognitive function and support needs. Early registration offers no advantage.
The pandemic highlighted these issues, particularly the need for full-time roles with proper compensation, but public attention has waned. These essential workers remain underpaid, undervalued, and under-resourced. We need continued advocacy to ensure we can provide the highest quality of care in long-term care homes.
RD: As we wrap up, I’d like to focus on the positive changes ahead. What initiatives are you most excited about?
SS: I’ll share two initiatives that really excite me. First: Dr. Jennifer Watt is creating a rehabilitation pathway for people with dementia. Traditionally, these patients are often excluded from inpatient rehabilitation due to ageist assumptions about their ability to participate. However, our pilot study has shown promising results that they can improve and return home successfully. We’ve now secured funding for a larger-scale study that could transform care for this growing population. When someone with dementia is hospitalized for something like pneumonia, they risk deconditioning, which can severely impact their ability to function independently at home. Proving the benefits of rehabilitation for these patients could fundamentally change how we approach their care.
Our second initiative addresses homelessness among older adults. In Toronto, 3,500 people over 50 use shelters nightly, and 35,000 seniors await supportive housing. Through our shelter outreach program, we’ve discovered that about two-thirds of the older adults we assess have undiagnosed dementia. Imagine managing dementia while moving from shelter to shelter. What’s particularly concerning is that while most of these individuals qualify for long-term care, less than 5 percent ever gain admission. We’ve recently received funding to work directly with older adults experiencing homelessness and their caregivers to create a new model of long-term care. This will be the first initiative worldwide to support transitions from shelter to long-term care, and we’re hopeful it will help address this critical gap in our system.
AV: One project I’m particularly excited about focuses on improving medical care in long-term care homes. Currently, residents face significant challenges attending outside medical appointments, and many unfortunately end up in emergency rooms, which can be particularly frightening and unsafe for older adults living with dementia. The pandemic highlighted how disconnected long-term care homes have been from our broader healthcare system.
The project has gained government support and is expanding. We’re now providing internal medicine consultations to long-term care homes and their primary-care providers, elevating on-site care capabilities including palliative and wound care. We’ve also implemented nurse-led outreach teams for on-site care to support medical care delivery within long term care homes. It’s encouraging to see Ontario Health embrace this initiative and provide funding support, which is showing real promise in transforming how we deliver care.
“Understanding what resources are available in your neighbourhood isn’t just about staying physically healthy—it’s about building connections and knowing where to turn for support.”
RD: Having supported so many people through these life transitions, what key advice would you offer to help families better prepare for aging?
AV: Echoing Sharon’s comments earlier, it’s crucial to have those important conversations early—establish your power of attorney, clearly communicate your wishes to your family, and ensure they understand your values and goals regarding aging and future medical care.
Second, from my rehabilitation perspective: stay active and engaged with your community. Take advantage of local exercise classes and programs. Understanding what resources are available in your neighbourhood isn’t just about staying physically healthy—it’s about building connections and knowing where to turn for support as your needs change.
SS: I completely agree with Ashley’s points. I’d also emphasize the critical importance of social connections. COVID-19 showed us how isolation affects older adults’ wellbeing. Regular social engagement and community check-ins should be a priority for everyone.
This post is presented for illustrative and discussion purposes only. It is not intended to provide investment advice and does not consider unique objectives, constraints or financial needs. Under no circumstances does this post suggest that you should time the market in any way or make investment decisions based on the content. Select securities may be used as examples to illustrate Burgundy’s investment philosophy. Burgundy funds or portfolios may or may not hold such securities for the whole demonstrated period. Investors are advised that their investments are not guaranteed, their values change frequently and past performance may not be repeated. This post is not intended as an offer to invest in any investment strategy presented by Burgundy. The information contained in this post is the opinion of Burgundy Asset Management and/or its employees as of the date of the post and is subject to change without notice. Please refer to the Legal section of this website for additional information.

